Hemorrhoids.
Everyone Has Them.
Literally.
Jon Potter, DO
Gastroenterology
Eau Claire GI Associates
Eau Claire
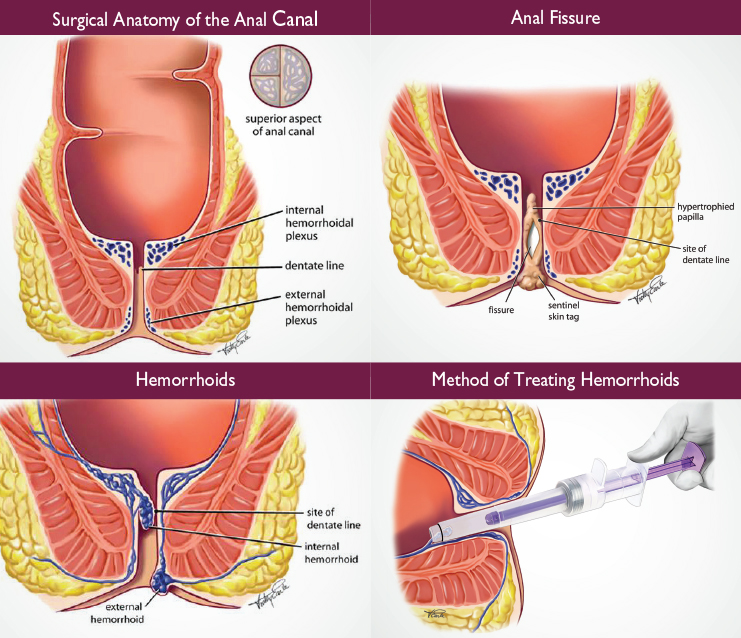
The vascular “cushions” that make up hemorrhoids are present normally in all individuals and act as a gasket, a seal, in the lower digestive tract. This, combined with the muscular sphincters, allows us to retain liquid and gas waste until a socially acceptable time. The hemorrhoids, arranged in three columns, also flatten to allow passage of solid waste. This complex structure, often taken for granted, does an incredible job in resisting infection and maintaining hygiene. When hemorrhoids become enlarged or inflamed and cause symptoms, they are then classified as “hemorrhoid disease”—essentially varicose veins of the rectum and anus.
Burning, Itching, Bleeding and Pain
Most patients with hemorrhoid disease experience some combination of these symptoms intermittently. Heavy lifting, diarrhea, and straining at hard stool may trigger a flare. Approximately 20% of adults are affected. Underlying risk factors include obesity, constipation, and pregnancy. Once present, the enlarged structures tend to persist and become bothersome from time to time. Complications include prolapse (falling out), blood loss, and thrombosis. The location of hemorrhoids determines their effect. Internal hemorrhoids are covered by thin rectal lining and may bleed severely. They have no sensitivity to pinch or burn. External hemorrhoids are a specialized type of skin that is very sensitive to pain. “Old” external hemorrhoids tend to close off and fibrose, forming skin tags. These generally do not need treatment. It is important to remember that any new blood, or darker red coloring in stool, should be evaluated for a different cause including a polyp or tumor. Treatment of the two types, or sites, of diseased hemorrhoids may be similar as the complex is a single vascular structure, crossing under the line between skin and gut lining.
OK, But It Really Hurts. What’s Going On?
 Surgical removal of the clot is sometimes needed. More commonly, the clot absorbs within 72 hours of onset. A doctor can help make the distinction between these problems and more typical hemorrhoid symptoms. More than one diagnosis may be present at the same time.
Surgical removal of the clot is sometimes needed. More commonly, the clot absorbs within 72 hours of onset. A doctor can help make the distinction between these problems and more typical hemorrhoid symptoms. More than one diagnosis may be present at the same time.
What Can I Do At Home?
Conservative therapy with diet and lifestyle modification is highly successful in the short and long term. Patients benefit from consuming at least 20 grams of fiber and drinking 1.5 to 2 liters of fluid daily. Alternatively, fiber supplements such as psyllium, wheat dextrin, and methylcellulose are easily consumed as an adjunct to a healthy diet. I advise patients to consume this fiber late in the day as part of their bedtime routine, integrated with tooth or denture care. Fiber delivered through the small bowel at night is less likely to cause bloating. Take one tablespoon of fiber, add water, stir with toothbrush, drink it, brush your teeth, go to bed. “Nature’s call” should be answered when possible, not delayed, with patience and avoiding straining. After a meal or cup of coffee colonic contraction occur, allowing a daily routine to become “regular”. Aerobic exercise, avoiding prolonged sitting, as well as refraining from lingering on the toilet are also of benefit.
What About All That Over-The-Counter Stuff?
Topical painkillers (lidocaine), anti-inflammatory steroids (hydrocortisone), and vasoactive agents (phenylephrine, diosmin, witch hazel, and others, which decrease fluid leakage and blood flow to enlarged vessels) are effective for external hemorrhoid irritation. Sometimes, that is the only treatment required. If there was a specific trigger, such as constipation, ask trusted healthcare professionals, including your pharmacist, and read product active ingredient labels.
Do not use non-prescription steroid products for more than one week, as side effects can occur. And don’t forget to pick up some disposable gloves for easy application. If problems are severe or persistent, a surgical hemorrhoidectomy may be necessary.
New Nonsurgical Treatments
In the past 10 years, hemorrhoid banding devices have become widely available for treatment of hemorrhoids right in the office. The techniques are heavily researched, safe, and effective. The procedure applies a small elastic band to an insensitive internal hemorrhoid, causing a cinching of the tissue. This heals and tacks tissue in place, reducing excess venous space and counteracting the stretching, enlarging issue of chronic internal hemorrhoids. External hemorrhoids can benefit as well.
What Is The Downside?
The banding procedure itself is very safe and comfortable. Patients may experience a moderate pressure sensation. Any pinch or pain is abnormal and should be evaluated. Minor bleeding may occur when the band, after the desired effect, sloughs off in 2 to 4 days. No treatment is effective 100% of the time. If banding does not achieve a satisfactory result, hemorrhoids may require surgery. That is the definitive treatment, once the diagnosis is certain and conservative measures have been tried. The potential complications of a band properly applied relate to pre-existing conditions. If you have Crohn’s Disease, colitis, a compromised immune system, weak connective tissue, or severe liver disease, please discuss your concerns with your provider.
How Many Treatments Are Needed?
Three on average, performed in two week intervals. The spacing of bands over three areas in the span of one month greatly reduces risk
of discomfort.
Is There Any Preparation?
None. No IV, enema, or laxative is needed.
Is It Covered By Insurance?
Generally, yes. Call the number on your card or document to inquire about provider networks and copay rates.
Who Can Perform Office-based Hemorrhoid Ligation?
Any well-trained provider, including gastroenterologists and surgeons.
Jon Potter, DO – Eau Claire G.I. Associates
For information or to schedule an appointment:
715-552-7303 | eauclairegi.com
Dr. Potter sees patients in Eau Claire, Chippewa Falls, Cumberland and Rice Lake.