|
Treatment of Knee Articular Cartilage DamageAustin Crow, MD How to know if you have a cartilage injury in your knee?
Because the above symptoms are not unique to cartilage injuries in the knee, it is important to have your doctor evaluate your knee. It is often as simple as an examination and getting an x-ray of the knee. For some injuries to the cartilage, it is necessary to obtain advanced imaging, such as an MRI or CT scan, to diagnose and assess the problem. Why is the cartilage damaged?There are many reasons the cartilage in your knee can be injured. In children and adolescents, the cause is most often a condition called osteochondritis dissecans, which occurs when a small area of the bone loses its blood supply and the overlying cartilage is damaged as this area of bone collapses. Another common cause in younger patients is a traumatic event often associated with other injuries to the knee, such as an ACL (anterior cruciate ligament) or meniscal tear. In this situation the bones in the knee have force placed across them resulting in a portion of either cartilage and bone or just cartilage being sheared off. As patients become older, the most common cause of cartilage damage is degenerative arthritis. This is when large sections of the knee have diffuse damage to the cartilage. The causes of degenerative arthritis are multifactorial, but can be attributed to attritional wear, malalignment of the leg, obesity or previous injury to the knee. Overall, degenerative arthritis is by far the most common reason patients will present to an orthopedic surgeon for knee cartilage damage. The CDC estimates that over 27 million Americans suffer from knee arthritis, with the prevalence increasing due to the obesity epidemic and aging of the “Baby Boomers.” Treatment
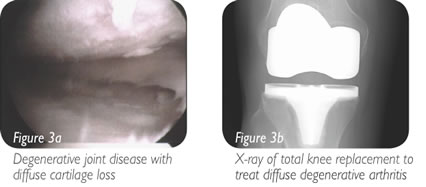
Generally treatment begins with conservative management including rest, non-steroidal anti-inflammatory medication, physical therapy and activity modification. These treatment plans are customized to the patient based on their exact condition. If this treatment plan fails to improve the patient’s symptoms, then surgical options are considered. The surgical techniques used to treat areas of damaged cartilage are largely based on the size of the lesion. The exception is with either osteochondritis dissecans or a traumatic injury, when there is a bone fragment with associated cartilage; these injuries are always repaired if possible. If the damage to the cartilage is in a focal area, the surgical options include different techniques to restore the cartilage surface. If the area is relatively small this can be accomplished by a technique called microfracture, where small holes are created in the bone, and a “cartilage scar” is formed. Small and intermediate sized lesions can be treated by transferring plugs of bone and cartilage from non-weight bearing portions of the knee to the damaged areas; this technique is call autologous osteoarticular mosaicplasty (Figures 1a and 1b). Autologous mosaicplasty cannot be used to treat larger lesions because there is only so much non-weight bearing cartilage available in the knee for transfer. If cadaver bone and cartilage plugs are used instead, this limitation is no longer an issue and larger lesions can be treated. Another option for treatment of larger lesions is grafting with allograft (cadaver) minced juvenile cartilage. In this technique minced pieces of cartilage are placed into the lesion and held in place by a biologic glue while it forms new cartilage. This technique is especially useful in treatment of articular damage to the patella (Figures 2a and 2b). Once the damage becomes so diffuse that a majority of the cartilage is involved, techniques to restore the cartilage are no longer effective and either portions of the joint or the entire joint can be replaced. If only one portion of the knee is replaced, it is called a unicompartmental (partial) knee replacement. If the entire knee is replaced, it is called a total knee replacement (Figures 3a and 3b). Both options are very effective at relieving pain and restoring function in the correct patients. Surgeons will often try to delay knee replacements in very young patients due to the concern for the artificial joint wearing out over time.
SummaryThere is a wide range of causes for patients to have damage to the articular surfaces of the knee. Their treatment often ultimately requires surgery and the surgical options are influenced by the cause of the damage, size of the lesion and the patient’s age. OakLeaf Surgical Hospital offers these advanced articular restoration procedures which offer significant improvements in pain and function.
Dr. Crow – Chippewa Valley Orthopedics & Sports Medicine |


 If you are having pain in your knee, it may be due to damage, either new or old, to the cartilage surfaces on the femur or tibia. You may experience pain at rest, but more often it is associated with activities such as labor, walking, exercises or sports. The knee may become swollen, especially after more vigorous use. Catching or locking during knee movement can also be present and is suggestive of a larger defect or loose flap of cartilage. Unfortunately, knee cartilage damage can occur in people of nearly any age, although the causes of the injury are highly variable.
If you are having pain in your knee, it may be due to damage, either new or old, to the cartilage surfaces on the femur or tibia. You may experience pain at rest, but more often it is associated with activities such as labor, walking, exercises or sports. The knee may become swollen, especially after more vigorous use. Catching or locking during knee movement can also be present and is suggestive of a larger defect or loose flap of cartilage. Unfortunately, knee cartilage damage can occur in people of nearly any age, although the causes of the injury are highly variable.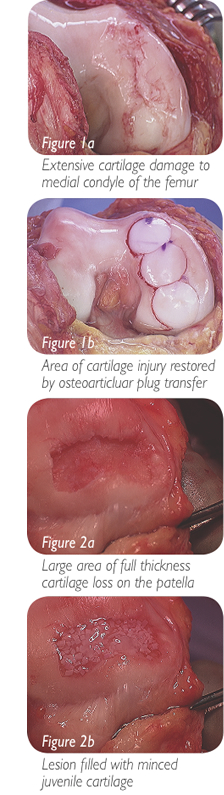 Because there are so many different causes of damage to the articular surfaces of the knee and patients can be of nearly any age, the treatment is highly variable. In addition, the treatment options are often based upon the size of the defect.
Because there are so many different causes of damage to the articular surfaces of the knee and patients can be of nearly any age, the treatment is highly variable. In addition, the treatment options are often based upon the size of the defect.