Mammography:
One size doesn’t fit all!
Richard Daniels, MD
General, Thoracic & Vascular Surgery
Evergreen Surgical
Eau Claire
The prognosis for breast cancer patients continues to
improve with early detection and advancements in treatment. Most women are aware of breast cancer and the need for mammograms. Wide-spread use of mammography has been credited with a significant reduction in deaths from breast cancer. Recent technology has improved mammograms with digital films and 3-D reconstruction (tomosynthesis). In general, the earlier you find breast cancer, the better the survival rates. Mammograms clearly help with early detection.
Most organizations such as the American Cancer Society and the American Medical Association recommend annual mammography beginning at the age of forty.
I also recommend liberal use of mammography for my patients.
 However, there are potential harms in having annual mammograms. Mammograms involve taking an x-ray of the breast. This exposes a woman to a very low dose of radiation. Most of the time, the risk is very low from the radiation. Mammograms also have a component of over-diagnosis that leads to over-treatment. Many biopsies are done unnecessarily because of the worry of “missing a cancer”. Mammograms have a false positive rate ranging from 20–63%. This suggests a lot of women undergo breast biopsies unnecessarily. Also a breast cancer can be diagnosed that may never become clinically apparent in one’s lifetime. One may not have had to endure treatment for this cancer because it would not have affected how long the patient would have lived. Finally, mammograms can lead to extra studies and appointments that can raise anxiety and stress levels for the patient. Many women are called back to radiology for “extra pictures”. Some are told that they need to see a surgeon after their mammogram has been reviewed. These are very anxious moments for most women.
However, there are potential harms in having annual mammograms. Mammograms involve taking an x-ray of the breast. This exposes a woman to a very low dose of radiation. Most of the time, the risk is very low from the radiation. Mammograms also have a component of over-diagnosis that leads to over-treatment. Many biopsies are done unnecessarily because of the worry of “missing a cancer”. Mammograms have a false positive rate ranging from 20–63%. This suggests a lot of women undergo breast biopsies unnecessarily. Also a breast cancer can be diagnosed that may never become clinically apparent in one’s lifetime. One may not have had to endure treatment for this cancer because it would not have affected how long the patient would have lived. Finally, mammograms can lead to extra studies and appointments that can raise anxiety and stress levels for the patient. Many women are called back to radiology for “extra pictures”. Some are told that they need to see a surgeon after their mammogram has been reviewed. These are very anxious moments for most women.
Two very large, well done studies have evaluated the benefits and harms of annual screening mammography. The United States Preventative Services Task Force (2009) and the Canadian National Breast Cancer Screening Study (2014) both have confused the issue as to the benefits of screening mammography. The study results question the guidelines for routine mammography between the ages of 40–59. The researchers concluded that “yearly mammography does not reduce breast cancer mortality (death) beyond that of physical exam”.
Despite these recent studies, most medical organizations still believe in routine mammography. I believe the benefits of mammography are REAL. What these studies do show is that “one size doesn’t fit all”. Some women may need to have mammograms more often than others. The frequency of future mammograms should be based on risk factors such as family history (first degree relatives with breast cancer etc.), genetics, and personal history (prior history of breast cancer). Women with more risk factors should be followed much closer with mammograms and self-awareness. Open discussions with your health care provider about mammography are vital to detecting breast cancers early. Better outcomes occur with improved communication between patients and their health care providers.
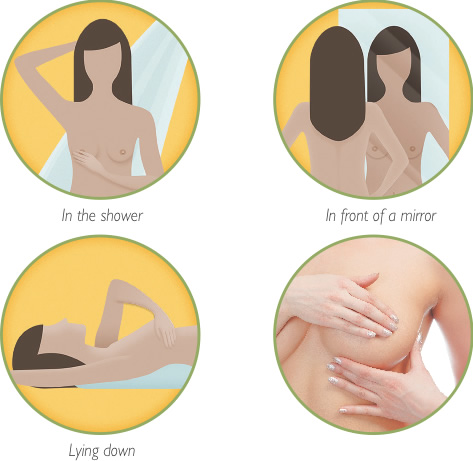
How to Perform a Breast Self-Exam
Dr. Daniels – Evergreen Surgical
For information or to schedule an appointment:
715-832-1044 | www.evergreensurgical.com
Dr. Daniels sees patients in Eau Claire, Chippewa Falls and Stanley.