|
Colon Cancer more common than you think!Brent Wogahn, MD Colon cancer is the second most common cancer for women and third for men. One out of every 20 people in the United States will have to deal with this type of cancer. It is also commonly known as “bowel cancer” and can also be called colorectal cancer if it involves the rectum. Risk Factors Colon cancer development is usually a very random event. While it is common, only 15% of colon cancers are genetically associated. Familial adenomatous polyposis and Gardner’s Syndrome are two examples of genetically transmitted precancerous polyps or growths in the colon. In both of these syndromes the colon is full of many polyps instead of the scattered few that most people with polyps develop. Consequently, they are at higher risk of colon cancer. Symptoms
Diagnosis
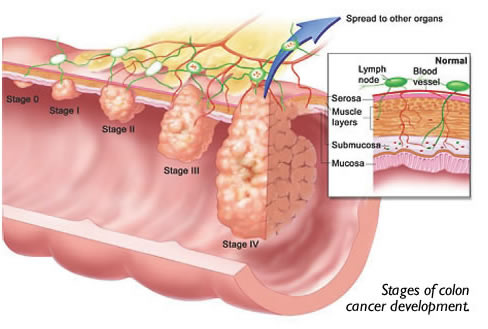
The mainstay of screening or diagnosis for colon cancer is a colonoscopy. That is a test done by Gastroenterologists and Surgeons using a lighted long flexible scope to look up into the rectum and colon directly. A bowel cleasing preparation must be done the day prior to the exam and sedation is used during the exam to make it more comfortable. The colonoscopy is very good at identifying small tumors or growths called polyps. A barium enema can also be used to screen for colon cancer. It can detect tumors and polyps greater the 1/2 cm in diameter, but does not allow for the suspicious item to be biopsied. Typically, I reserve this test for times when a colonoscopy was unable to be done or unable to be completed. Treatment Chemotherapy for colon cancer has been improving over the years with better survival statistics. Furthermore, we are treating more advanced non-obstructive cancers with chemotherapy and/or radiation prior to surgical resection. Thus hopefully causing the tumor to shrink and allow a better resection. However, chemotherapy is more typically employed after surgical treatment. Radiation therapy is used for low colon or colorectal cancers because of the adverse effects of the radiation on the small bowel. Colon cancer spreads via three modalities: direct extension, the lymphatic channels/lymph nodes and the blood stream. Tumor cells that get into the blood stream travel through the portal vein to the liver. This is why metastatic disease (spread of cancer) to the liver is common. Depending on the area in the liver, the number of metastatic nodules and the overall health of the individual, liver disease is more easily treated today. The nodules of cancer can be treated using microwave probes or cold freezing through the skin or during surgery. The nodules themselves may also be removed by surgery employing a new surgical device available locally that cooks the liver as we cut through it. This instrument essentially can make the surgery almost bloodless. I have even removed some tumor nodules laparoscopically using this device. Survival
Dr. Brent Wogahn – Evergreen Surgical |


 A special test card called “Stool Guaiac Card” can be used by your doctor to screen for occult blood (trace amounts) in the stool. Be aware that this test has many false negatives (you have cancer and the test says “no”) or false positives (no cancer, but the test says “yes”). The problem lays in the fact that many of the things that we eat or drink may mislead the test. Eating a special diet or rather not consuming particular items for three days prior to the test may help improve the accuracy of the results.
A special test card called “Stool Guaiac Card” can be used by your doctor to screen for occult blood (trace amounts) in the stool. Be aware that this test has many false negatives (you have cancer and the test says “no”) or false positives (no cancer, but the test says “yes”). The problem lays in the fact that many of the things that we eat or drink may mislead the test. Eating a special diet or rather not consuming particular items for three days prior to the test may help improve the accuracy of the results.