PAIN RELIEF —
LUMBAR SPINAL STENOSIS
Phillip J. Porter, MD
Neurosurgery
Brain and Spine Institute
Eau Claire
Generally, as we age most parts of our bodies become lax and loose. However, a common problem in older people is a tight spinal canal in the bones of the lower back called the lumbar spine. The spinal canal is a space in the middle of the bones through which the nerves for the legs, bowel and bladder run . Progressive degenerative changes, including bulging of the discs of the back, overgrowth of ligaments and formation of bone spurs (osteophytes) can narrow this canal, resulting in lumbar spinal stenosis. This condition may be present, but not cause symptoms for years or even decades, until the critical reserve of space in the canal becomes crowded. Thus, symptoms typically start after age 50. However, people who are born with a smaller than average size spinal canal may develop this problem at an earlier age.
The classic symptom of lumbar spinal stenosis is neurogenic claudication, which refers to pain, aching, fatigue, weakness (legs giving out) and numbness or tingling in one or both legs. Neurogenic claudication is caused by pressure on the nerves in the spinal canal when standing or walking. Standing straight up or leaning back causes tissues to buckle inwards and squeeze this space tighter, while sitting or leaning forward opens the space up. Patients often learn to walk with their bodies bent forward or to lean on something for relief while walking (such as a shopping cart). Many will have a long history of low back pain prior to leg symptoms. Typically the distance they can walk or amount of time they can stand gradually gets shorter, although sudden deterioration is possible.
Initially neurological testing of the legs is normal, but with time patients may develop persistent numbness, weakness and/or changes in reflexes. Imaging investigations may include plain X-rays, CT scan and MRI of the lower back to confirm the diagnosis and nerve or blood flow tests of the legs to rule out other medical conditions that may cause similar symptoms, such as peripheral neuropathy (deterioration of the nerves in the legs), hip or knee arthritis and especially vascular claudication (lack of blood flow to the legs due to atherosclerosis). High-resolution imaging (fig 2) allows the surgeon to determine exactly what tissue needs to be removed in the event that an operation is necessary.
The appropriate initial therapy of these conditions may include:
- Modification of activities
- Medications – including acetaminophen and anti-inflammatory drugs
- Physical therapy or chiropractic treatment
Surgery may be a good option for patients who have failed at least several months of conservative treatment or who develop numbness or weakness from the compression. The standard operation involves taking pressure off the nerves at one or more levels of the spine by removing the overgrown bone, ligaments and/or bulging discs (decompression), as well as possibly fusing the spine if there is severe associated back pain or loss of stability of the spine (decompression and fusion).
The XSTOP® interspinous spacer (fig 1) is a titanium device which is placed between the bones of the back to jack them up and prevent the in-buckling of tissue which occurs when standing or walking. This procedure is performed as an outpatient and may even be done under local anesthetic. Eighty percent (80%) or more of well-selected patients experience relief of leg symptoms with these surgical techniques. Low back pain is the symptom least likely to be improved by surgery.
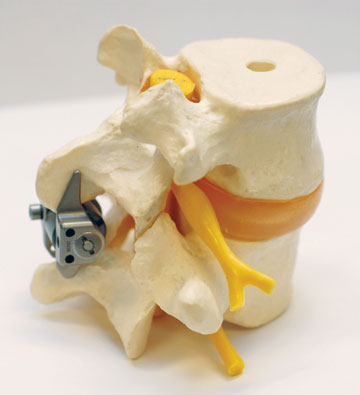
(fig 1)
The XSTOP® (Interspinous Process Decompression System), an interspinous spacer, is a titanium device which is placed between the bones of the back to “jack them up.
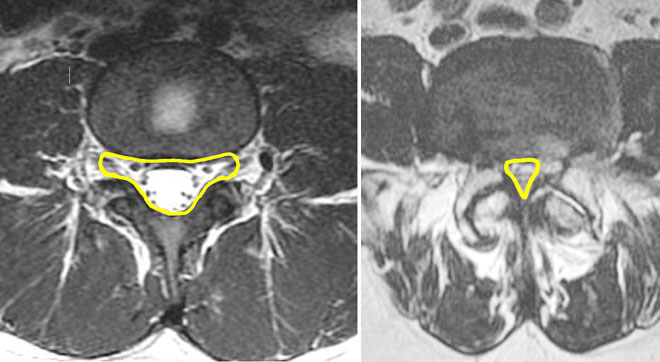
(fig 2)
High resolution imaging (MRI) allows the surgeon to determine what tissue has been impacted by stenosis. Image on left is of a normal spine. Image on the right is of a spine with severe stenosis.
For more information on treatment of lumbar spinal stenosis or to schedule
an appointment with Dr. Phillip Porter, Brain & Spine Institute, Eau Claire,
call 715.858.1777.